Women entering their mid-thirties experience significant physiological changes that require proactive health management. Understanding these shifts and implementing preventive strategies can dramatically influence long-term wellness, reduce disease risk, and maintain quality of life through the decades ahead.
Understanding the Transition: What Happens After 35

After age 35, women’s bodies begin the gradual transition toward perimenopause—the period leading up to menopause when hormonal fluctuations begin. Estrogen and progesterone levels start to decline, triggering changes that affect multiple body systems. This phase can last 4-8 years, causing irregular periods, mood swings, sleep issues, and fatigue.
The choices made during this critical window nutrition, exercise, stress management, and preventive screenings have profound effects on future health outcomes including cardiovascular disease, osteoporosis, and metabolic conditions.
Bone Health: Protecting Against Osteoporosis
The Estrogen-Bone Connection
Estrogen plays a pivotal role in maintaining bone homeostasis by regulating the balance between bone breakdown and bone formation. As estrogen levels decline during perimenopause and menopause, osteoclasts (cells that break down bone) become more active while osteoblasts (cells that build bone) slow down, tipping the scale toward accelerated bone loss. Research shows that up to 20% of bone loss can occur during the menopausal transition, and one in two postmenopausal women will develop osteoporosis.
Preventive Strategies for Bone Health

Calcium and Vitamin D Intake: Consume calcium-rich foods daily including milk, yogurt, kale, and fortified foods to maintain bone density. Adequate vitamin D is essential for calcium absorption and bone health.
Weight-Bearing Exercise: Engage in activities where feet and legs support body weight—walking, running, dancing, strength training—to stimulate bone formation and maintain density. Regular resistance training is particularly beneficial for preventing osteoporosis.
Bone Density Screening: Discuss bone mineral density testing with your healthcare provider, especially if you have risk factors such as family history, early menopause, or prolonged steroid use.
Cardiovascular Health: Addressing Increased Risk
How Menopause Affects Heart Health

Before menopause, women generally have lower cardiovascular disease risk compared to men, but this protection diminishes as estrogen levels fall. Estrogen helps control cholesterol levels, keeps blood vessels healthy, and prevents arterial plaque buildup. The menopausal transition is associated with adverse changes in blood lipid profiles, including increased LDL (bad cholesterol) and decreased HDL (good cholesterol), which elevate cardiovascular disease risk.
Additional changes during this period include weight gain (especially around the waist), elevated blood pressure, impaired glucose control, and increased fat accumulation around the heart—all contributing to heightened cardiovascular risk.
Cardiovascular Protection Strategies
Regular Health Screenings: Begin cholesterol screening at age 45 if no risk factors exist, or earlier if you have diabetes, family history, or other cardiovascular concerns. Monitor blood pressure regularly, as it may increase during perimenopause.
Heart-Healthy Nutrition: Adopt a plant-based diet rich in fruits, vegetables, whole grains, and healthy fats to support cardiovascular health and manage cholesterol levels.
Regular Physical Activity: Aim for at least 30 minutes of daily moderate exercise to maintain healthy weight, improve heart function, and reduce cardiovascular disease risk.
Avoid Smoking and Limit Alcohol: Smoking significantly increases cardiovascular risk, and excessive alcohol consumption can elevate blood pressure and contribute to weight gain.
Hormonal Changes: Management and Support
Recognizing Perimenopause Symptoms
Common symptoms during the perimenopause transition include irregular or heavy periods, hot flashes, night sweats, mood swings, anxiety, sleep disturbances, vaginal dryness, and decreased libido. Hormonal fluctuations can also lower stress tolerance and amplify existing mental health conditions.
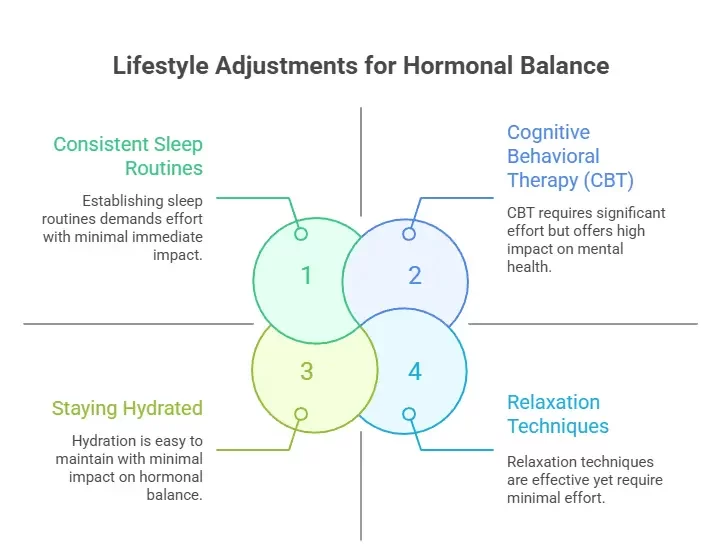
Lifestyle Adjustments for Hormonal Balance
Hormone Replacement Therapy (HRT)
HRT can effectively relieve hot flashes, night sweats, vaginal dryness, and improve sleep, mood, and joint pain. It may also reduce risks of osteoporosis, fractures, type 2 diabetes, and colorectal cancer. However, HRT carries potential risks including slightly increased breast cancer risk (depending on type and duration), blood clots, and cardiovascular events in certain populations.
Current medical consensus indicates that for healthy women with significant menopausal symptoms, the benefits of HRT typically outweigh risks, but individual factors must be carefully evaluated with a healthcare provider.
Essential Health Screenings After 35
Cancer Screenings
Cervical Cancer: Women ages 30-65 should receive Pap tests every 3 years, HPV testing every 5 years, or co-testing (both) every 5 years.
Breast Cancer: Mammogram screening recommendations vary, but many guidelines suggest starting between ages 40-50 depending on family history and personal risk factors. Women with elevated risk may need earlier or more frequent screening.
Colorectal Cancer: Begin screening at age 45 with colonoscopy every 10 years or annual stool tests.
Metabolic and General Health
Diabetes Screening: Monitor blood glucose levels, especially during perimenopause when insulin sensitivity may decrease.
Annual Well-Woman Visits: Schedule yearly preventive care appointments to review medical history, assess disease risk, discuss lifestyle modifications, and update vaccinations.
Comprehensive Lifestyle Recommendations
Balanced Nutrition: Prioritize whole foods, adequate protein, calcium-rich foods, and anti-inflammatory ingredients while limiting processed foods, caffeine, and spicy foods that may trigger symptoms.
Regular Movement: Combine cardiovascular exercise with strength training for bone health, heart health, weight management, and mood regulation.
Social Connection: Engage with family, friends, or support groups going through similar experiences to share strategies and reduce isolation.
Avoid Harmful Substances: Eliminate smoking and moderate alcohol consumption to protect cardiovascular and bone health.
Frequently Asked Questions
Q: At what age does perimenopause typically begin?
A: Perimenopause typically begins after age 35, though the average onset is in the mid-to-late 40s. It can last 4-8 years before menopause (defined as 12 consecutive months without a period).
Q: Can I prevent bone loss during menopause?
A: While you cannot completely prevent bone loss, you can significantly slow it through calcium and vitamin D intake, weight-bearing exercise, strength training, avoiding smoking, and limiting alcohol. Some women may benefit from medications or hormone therapy—consult your healthcare provider.
Q: Why does cardiovascular disease risk increase after menopause?
A: Declining estrogen levels remove the protective cardiovascular effects estrogen provides, including cholesterol regulation and blood vessel health. This hormonal shift leads to unfavorable lipid profile changes, increased blood pressure, weight gain, and impaired glucose metabolism
Q: What lifestyle changes are most important after age 35?
A: The most impactful changes include regular exercise (combining cardio and strength training), balanced nutrition rich in calcium and whole foods, stress management practices, consistent sleep routines, maintaining healthy weight, avoiding smoking, limiting alcohol, and keeping up with preventive health screenings.
Q: How can I manage hot flashes and night sweats naturally?
A: Wear light clothing, keep your bedroom cool, use fans, take cool showers, reduce stress, exercise regularly, maintain healthy weight, and avoid triggers like spicy food, caffeine, hot drinks, smoking, and alcohol. Cognitive behavioral therapy has also shown effectiveness for managing hot flashes.
Q: Do I still need regular health screenings if I feel healthy?
A: Yes—preventive screenings can detect diseases early before symptoms appear, when treatment is most effective. After 35, recommended screenings include cholesterol testing, blood pressure monitoring, cervical cancer screening, breast cancer screening (age-dependent), bone density testing (if risk factors exist), and diabetes screening.
Q: How does perimenopause affect mental health?
A: Hormonal fluctuations during perimenopause can lower your threshold for managing stress and amplify symptoms of anxiety or depression, especially if you have a history of these conditions. Sleep disruption from night sweats further impacts mood and cognitive function. Regular exercise, stress management techniques, adequate sleep, and professional support like CBT can help manage mental health during this transition.




